Abstract
Background Infections are a major cause of morbidity and mortality in CLL patients (pts), and COVID-19 pandemic has deeply emphasized the frailty of these patients. The systemic effect on the immune system induced by therapies and the intrinsic disease-related immune dysfunction are the main cornerstones in defining susceptibility to infections. It is well established that hypogammaglobulinemia and IGHV mutational status are factors associated with infection risk in CLL. Despite infection risk-assessment guidelines are available in clinical practice to guide an appropriate infection prophylaxis, to our knowledge an infectious risk assessment score system is not available in CLL to stratify patients.
Aims The aim of this study was to define a simple easy-to-use infectious risk score to facilitate clinical practice stratification of CLL pts, based on Binet stage, hypogammaglobulinemia (HGG), age and IGHV mutational status at diagnosis. We also aimed to identify the prognostic role of this model regarding the infection free survival (IFS) in a monocentric real-life cohort of CLL pts followed for over 25 years.
Methods We retrospectively evaluated 210 unselected CLL pts diagnosed from 1988 to 2018, with a median age at diagnosis of 64 years (range 37-88), distributed in 129 treated and 81 treatment-naïve at time of statistical evaluation (20-jul-2022).
During the course of disease 68 pts (32%) reported at least one severe infectious event (grade≥3 CTCAE), with need of hospital admission. We had previously found in our cohort that overall survival (OS) was heavily affected for pts that experienced an infectious event in during the first year before diagnosis, with higher mortality rate in pts with combined antibody deficiency (CAD) at diagnosis. Based on both these retrospective findings and already known infection-risk factors, we selected four easy-to-evaluate characteristics at diagnosis (Binet stage, HGG, age, IGVH mutational status), with the aim to predict the risk of severe infectious events. The next step was to assign a score between 0 and 3 to each item, based on hazard ratios in multivariate analysis (Cox proportional hazard regression model). We attributed scores as follows: unmutated IGVH (3 points), C Binet (3 points), age (2 points), low IgA level, lgG and IgM (1 point).
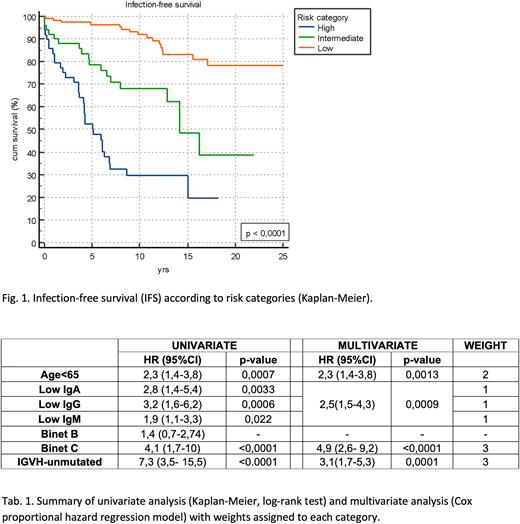
Results The median follow-up was 11.03 yrs. Age, IGHV mutational status, Binet stage and HGG were all statistically associated with IFS in both univariate and multivariate analysis (Tab.1). Finally, we identified a risk score for infectious events, grouped in three risk categories: low: 0-1; intermediate: 2-4; high: ≥ 5.
The 25-year IFS according to risk categories showed a median not reached for the low-risk group, 14.17 yrs for the intermediate group [(95%CI,12.86 to 1.21) HR 3.3 (95%CI,1.8 to 6.0)], and 5.11 yrs for the high risk one (95%CI,3.66 to 6.78) HR 8.4 (95%CI 4.2 to 16.9)] (p < 0.0001) (Fig. 1).
Conclusion Taking into account that this working model represents a single institutional effort based on a retrospective analysis, our score was able to predict a worse clinical outcome in terms of IFS in patients with high-risk score for severe infectious events. An appropriate screening for infectious risk at diagnosis could improve clinical management of CLL patients, defining both a fitter adherence to therapies and a better outcome, particularly in the COVID-19 era.
The application of this multiparametric model deserves further investigation and needs to be validated in prospective settings.
Keywords: Chronic lymphocytic leukemia, Immune deficiency, Infection, hypogammaglobulinemia
Disclosures
Murru:AbbVie: Other: Travel, Accommodations; Astrazeneca: Other: Travel, Accommodations; Janssen: Research Funding; Roche: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal